Fred Hutch Legacy Insiders
Winter 2024
Loyal supporters and their advisors are helping to accelerate discoveries that prevent, treat, and defeat cancer and infectious disease. We invite you to learn about the innovation their support makes possible.
Donor Spotlight: Debra Ramsey
Weaving a legacy for advances against colon cancer

“It just feels good to give,” says Fred Hutch supporter Debra Ramsey. “It feels good to know that I have an opportunity to make a difference.”
For Debra, including Fred Hutchinson Cancer Center in her estate planning is a powerful way to honor family members, friends and all those who have been affected by cancer. “I don’t think I could name three people who have not been touched by this disease,” she says.
That includes her late husband, Craig, who received treatment for cancer at Fred Hutch. From the minute they met in college, says Debra, his intelligence won her over. “I’m smart,” she laughs. “But Craig and his friends were ethereal.”
Read more
After Craig’s passing in 2020, Debra generously made several gifts to the Fred Hutch Family Resource Center, which provides a welcoming place for patients and families to learn about a specific diagnosis. During Craig’s treatment, she says, “The [Resource] Center was my oasis of calm.”
More recently, she began to look for a way to increase her giving. After talking with her son and daughter-in-law and the Fred Hutch Planned Giving team, she decided to include Fred Hutch in her estate and designate her gift to advance colon cancer diagnosis, treatment and care.
“I wanted the money to go to an institution that would be able to use it creatively to move research in cancer forward,” she says. “I cannot think of another place that my money would have had a greater impact to do good for people.”
To learn more about how you can make a legacy gift to Fred Hutch through your estate, contact us at 206.667.3396 or at plannedgiving@fredhutch.org.
2023: The Year in Photos
A look back at the important moments for Fred Hutch through photos

Everyone always says they had a busy year, and we believe them and agree. So did we.
In 2023, Fred Hutchinson Cancer Center established the new Division of Radiation Oncology, created a new referral-only Acute Clinical Evaluation Clinic and Sara Hurvitz, MD, took the reins as senior vice president of Fred Hutch’s Clinical Research Division and head of UW Medicine’s Division of Hematology and Oncology.
From physically expanding our patient care to sharing key findings at scientific conferences to gathering with community to help obliterate cancer, Fred Hutch’s researchers, clinicians and other employees saw many successes this year. We invite you to take a look at some of these achievements through our amazing photography.
We’ve also gathered together our most-read articles and two special story packages in case you missed them.
Read more
 The Research Administration Employee Engagement Committee hosted an Open House on May 16 on the Fred Hutch campus. This open house poster session showcased the work and collaboration of the 47 teams who support our science. Photo by Robert Hood / Fred Hutch News Service
The Research Administration Employee Engagement Committee hosted an Open House on May 16 on the Fred Hutch campus. This open house poster session showcased the work and collaboration of the 47 teams who support our science. Photo by Robert Hood / Fred Hutch News Service
 The waning of the pandemic allowed researchers, clinicians and others from across the organization to gather again to share ideas and strengthen working relationships. The Vaccine and Infectious Disease Division (VIDD) Faculty Retreat, pictured, was held in June. Photo by Robert Hood / Fred Hutch News Service
The waning of the pandemic allowed researchers, clinicians and others from across the organization to gather again to share ideas and strengthen working relationships. The Vaccine and Infectious Disease Division (VIDD) Faculty Retreat, pictured, was held in June. Photo by Robert Hood / Fred Hutch News Service
 Many organizations contributed to our efforts this year and their support was both appreciated and recognized. Here, an attendee of the 2023 Hyundai Hope on Wheels Ceremony, held at Fred Hutch in August, places a painted handprint on Dr. Scott Furlan’s lab coat. Photo by Connor O’Shaughnessy / Fred Hutch News Service
Many organizations contributed to our efforts this year and their support was both appreciated and recognized. Here, an attendee of the 2023 Hyundai Hope on Wheels Ceremony, held at Fred Hutch in August, places a painted handprint on Dr. Scott Furlan’s lab coat. Photo by Connor O’Shaughnessy / Fred Hutch News Service
 First Lady Jill Biden visited Fred Hutch in September, discussing the Biden Cancer Moonshot with Fred Hutch President and Director Dr. Thomas J. Lynch, Jr., and other scientists, and touring the lab of Dr. Cyrus Ghajar, a translational researcher working on an ambitious initiative to prevent metastatic cancer. Click on the photo to read more. Photo courtesy of Kariba Jack
First Lady Jill Biden visited Fred Hutch in September, discussing the Biden Cancer Moonshot with Fred Hutch President and Director Dr. Thomas J. Lynch, Jr., and other scientists, and touring the lab of Dr. Cyrus Ghajar, a translational researcher working on an ambitious initiative to prevent metastatic cancer. Click on the photo to read more. Photo courtesy of Kariba Jack
 Our clinical teams treated thousands of patients last year, helping families navigate cancer or undergo screening in order to catch the disease early. And they did it to an exceptional degree. Above, registered nurse Tiffany Curtis, left, receives a Daisy Award with colleagues in November. Photo by Robert Hood / Fred Hutch News Service
Our clinical teams treated thousands of patients last year, helping families navigate cancer or undergo screening in order to catch the disease early. And they did it to an exceptional degree. Above, registered nurse Tiffany Curtis, left, receives a Daisy Award with colleagues in November. Photo by Robert Hood / Fred Hutch News Service
 Diversity, equity and inclusion continued to be a significant focus for our organization. Above, Cierra Sisters founder and Fred Hutch research collaborator Bridgette Hempstead speaks during the Anti-Racism in Oncology video project premiere celebration. Click on the photo to read more. Photo by Robert Hood / Fred Hutch News Service
Diversity, equity and inclusion continued to be a significant focus for our organization. Above, Cierra Sisters founder and Fred Hutch research collaborator Bridgette Hempstead speaks during the Anti-Racism in Oncology video project premiere celebration. Click on the photo to read more. Photo by Robert Hood / Fred Hutch News ServiceMost-read articles of 2023
These five articles from 2023 were the top read stories on our website this year.
Insulin resistance turns tidy brain cells into slobs — which could be a link between diet and neurodegenerative diseases – Nov. 7
New work in fruit flies shows that a high-sugar diet impairs “housekeeping” brain cells.
Dr. Sara Hurvitz joins Fred Hutch, University of Washington – June 14
Longtime UCLA breast oncologist and international expert will be senior vice president of the Clinical Research Division.
Going long: Viruses linger with lasting impact – April 10
Herpes, HIV, Epstein-Barr and other viruses hang around, causing potential long-term health woes. Should ‘long COVID’ surprise us?
Dead to me? Insights into a tumor’s necrotic core – Feb. 27
Research from Cheung Lab reveals role for ‘dead zone’ within cancers as a launch system for metastatic spread.
Fred Hutch launches MET-X, a ‘transformative approach to metastatic disease’ – Feb. 3
New Center for Metastasis Research Excellence aims to detect, prevent, treat and cure stage 4 solid tumor cancers.
Special story packages
We also published two special story packages on topics relevant to our audience of cancer patients, caregivers, families and friends. Here are the links in case you missed them.
‘Cancer is a pain’ series
Pinpointing pain: Is it cancer or cancer treatment?
Peripheral neuropathy: When having no pain is a big problem
Bridging the pain communication gap: Patients, providers share tips
Cancer & Caregivers series
The challenges of cancer caregiving
Caregivers know compassion is critical; staying organized is, too
Insulin resistance turns tidy brain cells into slobs — which could be a link between diet and neurodegenerative diseases
New work in fruit flies shows that a high-sugar diet impairs “housekeeping” brain cells
 Neurons like it tidy. Brain cells called glia help neurons perform at their best by cleaning up toxic cellular debris. But a diet high in sugar makes glia insulin resistant — which turns them into apathetic housekeepers that let damaging debris pile up, according to new work from Fred Hutchinson Cancer Center scientists, published in the journal PLOS Biology. The findings in fruit flies could help explain how diet influences risk of neurodegenerative disorders like Alzheimer’s disease.
Neurons like it tidy. Brain cells called glia help neurons perform at their best by cleaning up toxic cellular debris. But a diet high in sugar makes glia insulin resistant — which turns them into apathetic housekeepers that let damaging debris pile up, according to new work from Fred Hutchinson Cancer Center scientists, published in the journal PLOS Biology. The findings in fruit flies could help explain how diet influences risk of neurodegenerative disorders like Alzheimer’s disease.
Read More
In the new work, Rajan Lab postdoctoral fellow Mroj Alassaf, PhD, confirmed that, like peripheral tissues, brain cells can become insulin resistant. Alassaf demonstrated that the high levels of insulin induced by excess dietary sugar causes glial dysfunction, which prevents glial cells from cleaning up damaging cellular debris.
“We found that it’s not about weight, it’s about insulin signaling,” Alassaf said.
While mid-life obesity has been linked to greater risk of later-life dementia, her findings suggest that it may be possible to keep brain cells healthy by focusing on improving insulin sensitivity.
A missing mechanism
Our diet, weight and metabolic health connect to our risks of other diseases, including cancer and neurodegenerative diseases, in ways that are difficult to untangle.
“Obesity is an independent risk factor for dementia, but the causative mechanism underlying that connection is largely unknown,” Alassaf said.
What is known is that malfunctioning of glial cells, which tidy up debris and influence neuron function by “pruning” nerve cells, can contribute to neurodegeneration. Studies have shown that changes in glial cell function can alter animals’ weight, metabolism and feeding behaviors. Whether glia can become insulin resistant, and whether this could cause changes in their function, was also unknown.
To study the effects of insulin on glial cells, Rajan and Alassaf turned to fruit flies. They’re an attractively simple organism in which to study how diet and adipose tissue influence health. Like us, fruit flies have an insulin-like hormone that helps regulate energy storage and energy-dependent behaviors like sleep, reproduction and food foraging. And like us, these tiny creatures bump up their lipid stores when they eat too much sugar for too long. (Yes, even fruit flies can eat too much sugar, although their exoskeletons limit the amount of new lipids they can amass.)
The time scale’s a little different, though: Flies become insulin resistant after just a couple of indulgent weeks. Insulin resistant cells need more insulin to wedge open the molecular “doors” that let sugar in. Insulin resistance is closely related to prediabetes and metabolic syndrome, and it’s a risk factor for developing type 2 diabetes and cardiovascular disease.
A team of Rajan Lab postdocs, including Alassaf, had already mapped out the timeline of flies’ “metabolic collapse” in a paper published last year in eLife. She decided to use the same experimental approach to study whether these diet-induced metabolic changes affect glia.
While insect glia and human glia aren’t exactly the same, glia in both organisms do the critical work of clearing up debris that can be damaging to neurons. These debris include cellular detritus released by neurons themselves, as well as the misfolded proteins that build up in neurodegenerative conditions like Alzheimer’s.
“What happens in these conditions is that glia become less efficient in clearing up these cytotoxic [cell-damaging] debris,” Alassaf said. “Leaving that debris behind induces inflammation, it induces secondary cell death — so clearing it up is a pretty crucial step in remedying damage.”

Too much sugar makes glia insulin resistant
Alassaf asked a simple question: If fruit flies spend a prolonged period eating a high-sugar diet known to make them obese, what happens to the insulin responsiveness of their glia?
In Rajan’s team’s previous study, the researchers had seen that flies developed insulin resistance in peripheral (non-brain) tissues after just two weeks of a diet containing 30% more sugar than normal. In the current study, Alassaf fed the flies the sugary diet for three weeks (about one-third of the average fly lifespan) and then compared the insulin sensitivity of their glia to the glia of flies that continued eating a standard diet.
Over time, flies overfed sugar increased their insulin levels to handle the extra sugar. Alassaf saw that despite this, their glia became less responsive to insulin than normal. The glia had become insulin resistant.
Glia use a cleanup protein called Draper to vacuum up nearby debris. After neuronal damage creates more debris, glia boost the levels of Draper to handle the extra cellular waste. Alassaf found that insulin-resistant glia had lower-than-normal levels of Draper, and that they didn’t ramp it up after nerve cell damage.
“We saw that at four days, when normal glia have done their job and cleared the debris, this neuronal debris persists much longer in flies with insulin-resistant glia,” Alassaf said.
As over-sugared flies’ insulin jumps, they also store the excess energy as fat, which can communicate with brain cells. To untangle the influence insulin and fat on glia, Alassaf genetically engineered flies to release extra insulin even when she kept the sugar in their diets at a normal level. This mimicked the insulin levels of flies eating a high-sugar diet — without the sugar. Alassaf showed that glia in these genetically manipulated flies turned down Draper. When she genetically manipulated fruit flies to keep their insulin levels low even when they ate excess sugar, their glia remained insulin sensitive, and Draper levels remained normal.
This shows that flies’ diet-induced glial dysfunction resulted from their insulin response, not their fat stores, she said.
A complex biological response to diet
The different timescales at which the brain and peripheral tissues become insulin resistant should inspire scientists to take a wider view of how diet affects health, Rajan said: “In humans, we think primarily of weight gain, but by increasing sugar in the diet, we’re impacting each cell differently.”
Alassaf’s next steps will be two-pronged. First, she’ll continue exploring the biology behind insulin’s effects on glia. Insulin-resistant glia appear to experience a shift in how they generate energy, which could prevent their activation. In the previous work, Rajan’s team had showed that certain lipids are more toxic to health than others. Glia also store lipids, and Alassaf wants to see how these lipids affect glial and neuronal function.
She also wants to test how insulin-resistant,impaired glia affect fly behavior. While flies don’t get dementia, she test whether insulin resistance in their brain affects their performance on tests of learning and memory, and whether improving their insulin sensitivity can also improve their scores.
The good news for anyone who’s worried about how mid-life obesity or weight gain may affect their risk of dementia later is that insulin resistance is reversible, Rajan noted. It can be improved with changes to dietary and activity habits. There are already hints that medical interventions that improve insulin sensitivity, like the diabetes drug metformin, can protect against dementia — and Alassaf’s work supports investigating this further, Rajan said.
“As a scientist, what you want to do is not just find a cause, but also provide an intervention,” she said.
This work was funded by the National Institute of General Medical Sciences, the McKnight Foundation and the Helen Hay Whitney Foundation.
Sabrina Richards, a staff writer at Fred Hutchinson Cancer Center, has written about scientific research and the environment for The Scientist and OnEarth Magazine. She has a PhD in immunology from the University of Washington, an MA in journalism and an advanced certificate from the Science, Health and Environmental Reporting Program at New York University. Reach her at srichar2@fredhutch.org.
Are you interested in reprinting or republishing this story? Be our guest! We want to help connect people with the information they need. We just ask that you link back to the original article, preserve the author’s byline and refrain from making edits that alter the original context. Questions? Email us at communications@fredhutch.org
What’s new in breast cancer research? SABCS 2023 takeaways
New drug combos for metastatic patients and a strong focus on toxicities at San Antonio Breast Cancer Symposium
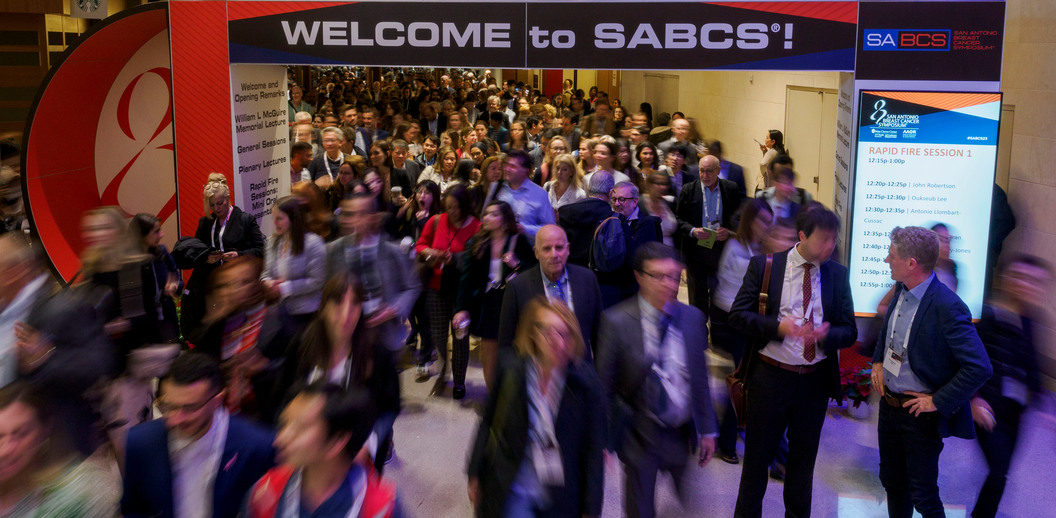
Scientists, oncologists, patient advocates and a host of others dedicated to stopping the second leading cause of cancer death in the U.S. gathered in Texas last week for the 46th San Antonio Breast Cancer Symposium.
The world’s leading breast cancer research meeting, SABCS 2023 drew approximately 10,000 attendees, with researchers sharing more than 1,700 new scientific abstracts and, hopefully, far fewer germs.
Physician-scientists and others from Fred Hutchinson Cancer Center presented via podium and poster, with findings on everything from new drug combinations to help patients with HER2 positive metastatic disease live longer to new ways to identify which patients are most likely to skip their helpful but often unpleasant anti-hormone medications.
Read More
Precision treatment and de-escalation were ongoing themes, with researchers and patients both advocating for individually tailored treatment and a “less is more” mindset when it comes to financially and physiologically toxic therapies. As usual, researchers shared a raft of results from several large clinical trials including monarchE, PROSPECT, KEYNOTE and IDEA, the latter looking at anti-hormone therapy alone after lumpectomy for post-menopausal women.

Hope for patients with HER2+ brain mets
Sara A. Hurvitz, MD, FACP, senior vice president and director of Fred Hutch’s Clinical Research Division and professor and head of UW School of Medicine’s Division of Hematology and Oncology, presented new data from HER2CLIMB-02 during one of the first general sessions.
The trial looked at a new drug combo for metastatic HER2+ breast cancer patients. It was noteworthy for its large recruitment of patients with metastasis to the brain and received wide media coverage.
“This is the first time that tucatinib [also known as Tukysa] has been evaluated with an antibody drug conjugate in a phase 3 randomized trial,” Hurvitz said. “And nearly half of the patients had brain metastases.”
The first HER2CLIMB trial resulted in the 2020 approval of the drug combination tucatinib, trastuzumab and capecitabine (also known as Xeloda, a chemo agent) by the U.S. Food and Drug Administration.
“HER2CLIMB showed that the use of tucatinib, which has the ability to penetrate the blood brain barrier, was associated with an improved survival for all patients including those with brain metastases,” Hurvitz said.
Investigators then went on to try additional tucatinib-based combinations.
The phase 3 trial HER2CLIMB-02, which included more than 450 patients with locally advanced or metastatic HER2+ breast cancer, looked at the efficacy of combining tucatinib and trastuzumab emtansine, sold as Kadcyla or T-DM1. Trastuzumab (Herceptin) was one of the first targeted treatments for HER2+ breast cancer.
Patients received either tucatinib plus T-DM1 or placebo plus T-DM1. Median progression free survival for those in the combo arm was 9.5 months; those in the placebo plus T-DM1 arm had 7.4 months. Median progression-free survival for patients with brain mets who received the combo was 7.8 months; patients with brain mets in the other arm had 5.7 months.
Hurvitz said the findings showed a “statistically significant” improvement in progression free survival in overall patient population and a strong trend in improvement in the patient population with brain metastases.
“Combining HER2+ directed therapies can improve patient outcomes in this disease setting,” she said. “HER2-positive breast cancer has a predilection for spread to the brain and when this occurs, prognosis is poor. Few options exist for the successful management of breast cancer brain metastases, making this an area of unmet need.” Watch Dr. Sara Hurvitz share trial results in this ASCO Post video.
The HER2CLIMB trials, which are ongoing, are funded by Seagen, Inc. in collaboration with Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc.
Promising drug combo for triple positive mets
Hurvitz and Fred Hutch breast oncologist Hannah Linden, MD, FACP, associate program director of the Medical Oncology and Hematology Fellowship Program at Fred Hutch and UW Medicine, were also part of a phase 2a investigation of the bispecific monoclonal antibody Zanidatamab in combination with the CDK4/6 inhibitor palbociclib (Ibrance) and the anti-hormone drug fulvestrant (Faslodex) in patients with HER2+ and ER+, or triple positive, metastatic breast cancer, or MBC.
Added as a late-breaking abstract, the trial enrolled 51 participants and accepted previously treated patients with stable brain metastases, according to Hurvitz, senior author.
“We’re looking at Zanatatinab, which targets HER2 at two different locations, in combination with a CDK4/6 inhibitor and anti-hormone therapy, and the efficacy results are exciting,” she said. “The responses we’re seeing and progression free survival are pretty good for patients who’ve had a median of four lines of therapy.”
The trial, which is ongoing, found the drug combo offered a median progression-free survival of 12 months in the overall population and 15 months in those with centrally confirmed HER2+ disease, with a median duration of response lasting 15 months.
Researchers charactered the drug combo as “well-tolerated with an easily manageable safety profile.” Most adverse events were mild. The most common moderate to severe treatment-related adverse effects included neutropenia, anemia and low platelets — side effects known to be associated with palbociclib (Ibrance).
Researchers believe the results support further development of non-chemotherapy treatment regimens for this group of patients.
“I think these are very promising data,” Hurvitz said.
Sponsor for this trial is Jazz Pharmaceuticals.
Who is more likely to stop anti-hormone therapy?
Health services researchers Scott Ramsey, MD, PhD, and Joe Unger, PhD, MS, from the Hutchinson Institute for Cancer Outcomes Research worked with lead author Dawn Hershman, MD, MS, of Columbia University Irving Medical Center, and others on a SWOG Cancer Research Network study that created a risk model to predict which breast cancer patients will likely stop taking their anti-hormone medications.
Presented by Hershman in a poster spotlight discussion session, the study focused on ER+ breast cancer patients who are prescribed anti-hormone medications as part of their regimen. Research shows many women stop taking the daily pills — mainly due to unpleasant side effects like joint pain and hot flashes — increasing their risk of recurrence.
Researchers looked at non-clinical factors associated with non-adherence such as demographic and socioeconomic factors, creating a risk model with data from a previous SWOG trial. A total of 724 patients were registered from 40 institutions. More than half (64.5%) had been on aromatase inhibitors, also known as AIs, for less than a year before registration. Observed adherence after three years was 35.9%.
Nonadherence was associated with an urban environment, especially living in a large city; a younger age; a lack of college education and minimal out-of-pocket cost for the medication. Race and ethnicity data were not associated with non-adherence.
“These findings provide further evidence that an individual’s social and economic background can contribute vital information in predicting the course of their treatment,” said Unger, senior author on the study. “This recognition is important for establishing early on which patients are at much greater risk of non-adherence to long-term AI therapy, which could allow more effective targeting of interventions.”
Funding came from the NCI and in part by the Conquer Cancer Foundation and the Breast Cancer Research Foundation
Creating trusted messages with community partners
Researchers on the FOR ME project, aimed at “Fostering Opportunities in Research through Messaging and Education,” also presented a poster update. Investigators on the study include Fred Hutch public health researcher Vida Henderson, PhD, PharmD.
Launched in 2022, FOR ME is developing, optimizing and testing out a narrative decision aid — in this case, a web-based video, for Black women diagnosed with breast cancer. Its end goal is to produce a video promoting shared decision-making and clinical trial participation, based on information gleaned from interviews and story circles with community members.
Researchers have conducted interviews with patients and advocates, community members, clinical trial office personnel and others, identifying what helped and what hindered people to join trials. Next steps include creating a culturally sensitive script and set of storyboards, testing them out on focus groups and then incorporating their feedback. The video will then be produced and test piloted with patients newly diagnosed with cancer.
Henderson said community-based participatory research was crucial to the project.
“Underrepresentation of Black patients in cancer clinical trials slows scientific advancements,” Henderson said. “The involvement of community partners in protocol development, data collection and dissemination — including Black women with breast cancer, the end-users of this video/decision aid — resulted in more culturally responsive, sensitive, impactful and relevant interventions.”
Funding came from the American Cancer Society and the V Foundation, among other sources.

Understudied breast cancers and better communication
Additionally, Fred Hutch patient research advocate Lynda Weatherby and collaborators presented a poster calling attention to the risk young mothers face if they are diagnosed within 10 years of having a child. Postpartum breast cancers are more likely to become metastatic, so adherence to treatment — and clear communication and education — is key.
Other highlights from the annual conference included new research on lobular breast cancer, a subtype that affects up to 15% of patients and presents special challenges due to its tendency to grow in strands, rather than clumps (making it difficult to image). The subtype was highlighted in a long-awaited mainstage educational session as well as dozens of posters, including one highlighting a new genomic driven artificial intelligence system that can detect mutations that drive this disease.
SABCS 2023’s many patient advocates also provided crucial reminders about clear communication between patient and provider.
“Doctors should listen to their patients,” said MBC patient advocate Sheila McGowan during a session on side effects. “Make sure you’re asking about the side effects. Make sure your patients know what a side effect is — some patients don’t even know!”
Patients may also be afraid to tell their doctors about side effects, she added, because they’re worried they’ll be taken off the treatment.
“Make sure patients know that dose reductions are a possibility,” she urged.
Is it safe to de-escalate treatment?
The de-escalation of toxic treatments (and/or their equally toxic price tags) was the subject of several posters and presentations including the following:
- Certain early breast cancer patients can safely skip radiation after lumpectomy, or breast-conserving surgery (BCS), per results from PROSPECT, an Australian precision therapy trial that used presurgical MRI and postsurgical tumor pathology to rule out toxic treatment and boost quality of life.
- The Patient-Centered Dosing Initiative, led by MBC patients, presented survey data from 1,200+ patients and 119 U.S. oncologists highlighting the need for tailored dosing. The poster, shared in an education session, concluded “patient-centered dosing discussions should be part of routine care and may consequently improve quality of life.”
- Fred Hutch patient research advocate Teri Pollastro and collaborators shared the design for STOP-HER2, a phase 2 clinical trial investigating whether HER2+ MBC patients can stop taking trastuzumab (Herceptin) in a poster spotlight presentation. Currently recruiting “exceptional responders” to anti-HER2 therapy at 10 U.S. cancer treatment centers, the trial will follow (and evaluate) patients who continue and patients who stop anti-HER2 therapy.
- Oncologists also shared both pro and con arguments for the use of anthracyclines, a common chemotherapy drug for breast cancer. On the plus side, they’re affordable and efficacious (especially in developing countries); on the other hand, they have serious (but rare) toxicities including heart damage, congestive heart failure and leukemia.
Throughout the five-day event, patient advocates and physician-scientists alike shared reminders about not using subjective or minimizing language when presenting clinical trial results, particularly when relaying the tolerability of side effects.
“While attending SABCS 23, please beware of the terminology ‘manageable and tolerable’ when it comes to side effects,” the non-profit Advocates for Collaborative Education, or ACE, posted on social media mid-conference. “Please ask yourselves, ‘Manageable and tolerable to WHOM?’”
Diane Mapes is a staff writer at Fred Hutchinson Cancer Center. She has written extensively about health issues for NBC News, TODAY, CNN, MSN, Seattle Magazine and other publications. A breast cancer survivor, she blogs at doublewhammied.com and tweets @double_whammied. Email her at dmapes@fredhutch.org. Just diagnosed and need information and resources? Visit our Patient Care page.
Join the Thomas Legacy Society
The Thomas Legacy Society at Fred Hutch is a special group of supporters who have made a commitment through a legacy gift to drive lifesaving cancer research and improve the lives of patients in the years to come.
What does a unique gift like this actually do? By making a gift to Fred Hutch in your will or trust, or by naming us as beneficiary on one of your financial or investment accounts, you contribute to:
- Research for discovering how to prevent, detect, and treat cancer and related diseases.
- Upgrades to existing technology and acquisitions of new equipment.
- A variety of assistance and support for patients and their families.
- Staff and researchers who further the cause of curing cancer faster.
Visit our website to learn more or contact us.
Already included Fred Hutch in your estate plans? Please let us know so we can ensure your wishes are carried out as you intend!



