Fred Hutch Legacy Insiders
Learn how loyal supporters and their advisors are fueling breakthroughs in research for cancer and related diseases that impact patients worldwide. We hope you enjoy these stories.
A family commitment to breakthrough science
For Doug Smith and Mary Templeman-Smith, giving to Fred Hutch is a powerful way to honor loved ones and support care and cures.
 “The [fund] is so flexible,” said Doug. “You can keep your financial advisor, have them manage the money, or you can choose funds managed by the donor advised fund.” — Doug Smith
“The [fund] is so flexible,” said Doug. “You can keep your financial advisor, have them manage the money, or you can choose funds managed by the donor advised fund.” — Doug Smith
In a way, donor Doug Smith actually helped build Fred Hutchinson Cancer Center – literally. Doug and his wife, Mary Templeman-Smith, first got to know the organization when Doug was chief financial officer for University Mechanical Contractors (now known as UMC), a firm that helped plan and build the Hutch’s state-of-the-art Seattle campus. Over time, he became familiar with the Hutch’s research, and impressed by the integrity of its scientists and staff.
“We got to meet a lot of the doctors,” shared Doug. “We got to hear about the passion for the cures and the patients.” The couple’s connection with Fred Hutch “evolved through watching really, really good people talk about the things that we can do better,” he said. “And it was like, ‘Wow, I can’t do what they can do, but I can give dollars.’ And that helps.”
Read more
Making a difference
“Cancer has and will touch all of us,” shared Doug. “My sister lost her fight at 61. She didn’t get the benefit of the Hutch. … We just want to be part of making that expertise as available as we can.”
“We’ve also had friends that have gone through treatments for lymphoma and multiple myeloma. … So, we have that connection,” added Mary. “We have been very blessed with success in our life, with our family and business, so we want to share.”
For Doug and Mary, writing checks at fundraising events gave way to a desire for a more intentional giving approach. A donor advised fund made that possible.
Donor Advised Funds at Work
Donor advised funds allow an individual to set aside cash, property, stock, or other assets, receive a tax credit immediately, and then recommend grant money to nonprofits over time.
For the Smiths, setting up a donor advised fund was “intentional, methodical, and practical.” It was also powerful — giving them a new way to simplify their philanthropic giving and deepen their impact on lifesaving cancer research. In fact, Doug and Mary are not only making gifts to the Hutch from their fund during their lifetime, but have included the Hutch as a beneficiary of the fund as part of their estate planning.
“The [fund] is so flexible,” said Doug. “You can keep your financial advisor, have them manage the money, or you can choose funds managed by the donor advised fund.” He added that it also simplifies tax reporting – turning sheafs of receipts into “one little piece of paper.”
A family relationship
Now, the Smiths are planning to continue what has become a family relationship with Fred Hutch. One of their daughters, Lauren Smith, and her fiancé, Cam Lamarche, are part of the Hutch’s Innovator’s Network, which welcomes young professionals to build community and support cancer research. For their part, Doug and Mary are inspired not only by the Hutch’s established researchers, but by the passion of early career scientists. “It’s about making a difference,” said Doug. “And who doesn’t want to support their kid’s careers, their friends’ children’s careers, and the early career scientists setting out to change our world?’
“You know, it just makes me humbled to hear researchers talk about what they do,” he added. “Donating is the part I can do.”
Want to learn more about donor advised funds and how this giving option can work for you? Feel free to contact PlannedGiving@fredhutch.org for more information.
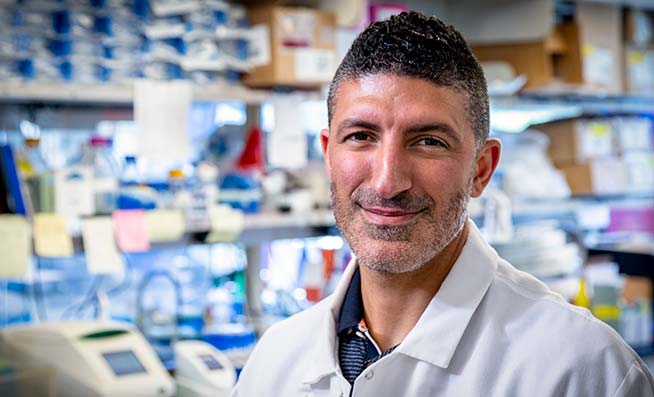
Understanding the mechanics of breast cancer metastasis
Ghajar Lab research reveals why muscle tissue doesn’t get mets, how dormant tumor cells in the breast wake up and proliferate
 Breast cancer in the breast doesn’t kill you: It’s breast cancer that’s traveled out of the breast and into a friendly microenvironment within some organ system — your bones or lungs or liver or brain — where it begins the unchecked cell growth that will eventually become a metastatic tumor.
Breast cancer in the breast doesn’t kill you: It’s breast cancer that’s traveled out of the breast and into a friendly microenvironment within some organ system — your bones or lungs or liver or brain — where it begins the unchecked cell growth that will eventually become a metastatic tumor.
That’s the breast cancer that kills you.
Read more
Not all patients develop metastatic breast cancer, or MBC. But research at Fred Hutchinson Cancer Research Center in Seattle found that 20% of early-stage breast cancer patients will develop metastasis, also known as stage 4 or secondary cancer, within 20 years of their original diagnosis.
There are currently many therapies, but no cures for metastatic disease. There’s also no consensus as to why some patients develop “mets” and some don’t, although scientists do know that not all cancer cells that escape a primary cancer site automatically become distant metastatic tumors.
But two new studies from the Hutch’s Ghajar Lab, one published this week in Nature Cell Biology (and another in the January 2022 issue of Nature Cancer), have provided intriguing answers to key questions about metastatic disease.
Why do some dormant cells wake up and start growing tumors in our brains or other organs while other dormant cells stay quiet? Why is the tissue in our lungs friendly to cancer proliferation while other tissue, like that in our muscles, is hostile to metastatic disease?
Read on for new findings. And expect more to come, as translational researcher Dr. Cyrus Ghajar and his team delve into the mechanics — and potentially exploitable vulnerabilities — of breast cancer metastasis, the breast cancer that kills.
Why don’t muscles get mets?
Metastasis is not a given. Our body’s immune system destroys most of the cancer cells that leave a tumor site. And some tumor cells become so comfy in their tiny microenvironment niches, they stay dormant — harmlessly asleep — and never wake up to start their deadly proliferation.
Autopsies performed on breast cancer survivors who’ve succumbed to something else have revealed slumbering cancer cells in their bone marrow or livers or brains. Autopsies have also revealed single tumor cells in the muscle tissue of MBC patients, but metastatic tumors in muscle tissue are quite rare.
Dr. Sarah Crist, a former graduate student in the Ghajar Lab who is now a postdoctoral fellow at the University of Minnesota, teamed up with Ghajar and others at the Hutch as well as researchers in Colorado and Australia to learn why muscles don’t seem to develop metastatic tumors. They discovered at least one process by which muscle tissue is able to keep disseminated tumor cells from growing into tumors: by completely stressing them out.
“One thing that’s unique about muscle is it’s a highly metabolic organ,” Crist explained. “It contracts all the time and it takes a lot of energy to make it function. It’s incredibly active and because it’s so active, it needs to be constantly building energy.”
Crist and colleagues wondered if the metabolic nature of muscle was somehow related to the harsh environment it presents for metastatic cancer growth.
“Our hypothesis was that the muscle was consuming something, so that something was no longer available for the tumor,” she said.
What they found was that metastasis was not able to form because the tumor cells were too stressed out by oxidants — reactive molecules that can cause damage in the cell — as part of an essential and intricate cellular process called redox metabolism.
“Muscle deprives tumor cells of antioxidant building blocks while simultaneously putting them under high oxidative stress,” said Ghajar, co-author on the study. “It’s a bad combination.”
Disrupting the balance
Using mice, organotypic culture models (a recreation of a human tissue in a petri dish) and metabolomic profiling, which captures the unique chemical fingerprints specific cellular processes leave behind, the researchers traced various molecular pathways to discover that skeletal muscle imposes a sustained oxidative stress on disseminated tumor cells which impairs their ability to proliferate.
“We found these tumor cells are immediately stressed upon traveling to the muscle,” Crist said. “It’s like their balance is off in terms of the redox metabolism — they can’t get past the single-cell stage because the environment is so stressful. They basically don’t have the ability to do anything but survive. They’re using all of their resources just to live in this harsh environment.”
The scientists validated their finding in multiple ways, including by giving tumor cells additional antioxidants.
“That’s the only time we saw the disseminated tumor cells grow in muscle tissue,” she said. “We gave them an extra dose, a much higher amount than is normally present.”
Scientists, of course, are not trying to find new places to grow metastatic tumors. The idea is to identify whatever it is that makes muscle tissue unfriendly to cancer, then use that information to make welcoming environments — like the lung, the liver, the brain and other organs — more hostile.
In their studies they were able to do just that, slowing the proliferation of disseminated tumor cells in the lung by disrupting the delicate balance of redox metabolism, subjecting them to the exact amount of oxidative stress that they experience in skeletal muscle.
“When we did this, we showed profound growth suppression in lung tissue,” Ghajar said. “And if they pushed the cancer cells even further, they died, suggesting a new vulnerability of disseminated tumor cells that can be exploited in patients.”
Of mice and men and women
But patients aren’t mice. Can they do this in people?
“That is the question,” said Crist, recent winner of the Hutch’s Harold M. Weintraub Graduate Student Award. “We’re thinking about how we would administer something that would be more oxidative, to make the tumor cells more stressed. But it’s all about finding the sweet spot — that ‘Goldilocks amount’ — not too much, not too little. You need to stress out the cancer cells without stressing out the body.”
And it’s not necessarily outright cell death they’re after: It’s redox imbalance.
“If you can create enough imbalance, you can stop these cells from growing,” she said. “It might be more realistic to make them stable, to keep them dormant. We don’t know at this point what to give to people, but we know this is a vulnerability we can try and target.”
Ghajar said his lab is working toward putting a clinical trial together to test the theory out.
“Our lab is trying to get to the bottom of the tissue-specific mechanisms of dormancy,” he said. “The hope is at some point that even though the players — the cells and the molecules — are different, maybe they converge on a common theme, providing a means by which one can keep these cells asleep throughout our body.”
How do brain mets get started?
Metastasis in the brain starts like other mets: Single cancer cells or tumor cell clusters travel there, just as they travel to other organs in the body, and if they make it to the brain alive, they soon become dormant, sometimes for months, sometimes for years or even decades.
In a certain segment of people, though, something rouses these sleeping cells and signals them to start dividing.
Approximately 15% of all MBC patients go on to develop brain metastasis, although it’s more common in those with HER2-positive or triple-negative disease (around 30% of metastatic triple-negative breast cancer patients get brain mets). New cancer therapies have helped MBC patients live longer but living longer also means the cancer has time to travel to the brain and set up shop. Incidence of MBC brain metastasis has increased over the last 10 years.
Brain mets are painful, debilitating and often fatal. The blood-brain barrier, a network of blood vessels and tissue made up of closely spaced cells that keep harmful substances (think pathogens) from reaching the brain, makes it difficult to deliver drugs. And MBC tumor cells are adept at outsmarting our body’s immune system. Therapies to either prevent or treat these cancers are desperately needed.
But a deep understanding of the process — the whole metastatic cascade — is also necessary.
Another paper from the Ghajar Lab, published in Nature Cancer in January, provided key insights into how these tumor seeds reawaken and begin to spread in the brain — a process that has largely gone without study.
It also offers hints as to how they might be stopped.
“This is the first study to show that dormancy is the rate-limiting step of brain metastasis,” Ghajar said. “Which means that we should be focused on dormancy and preventing metastasis by targeting these dormant disseminated tumor cells. From this point, it’s a long way to where you have something that will impact patients, but you have to start somewhere.”
A window into the world of brain mets
Led by Dr. Jinxiang “David” Dai, the research team (which included Ghajar, other Hutch scientists and partners from institutions in California, Colorado, New York, Pennsylvania, Utah and Germany) used “serial intravital imaging” — a literal window installed into the brains of living mice — to watch how single cancer cells escape from a dormant state within the brain’s microenvironment and begin to grow and spread as deadly tumors.
“We wanted to know, on a more granular level, what these dormant cells were doing,” Ghajar said. “Are there clusters of cells? Single cells? Are they growing slowly over the course of years? Are they dividing every two weeks, every four weeks, every week? No one had watched the cells that can form brain metastasis as they come into the brain and contrasted them with those that can’t to see where they differ.”
Dai, Ghajar and teammates installed intravital windows into live mice in order to witness the progression — or lack thereof — of metastatic triple-negative breast cancer cells in the brain. Some of the cells were dormant and some were selected for their ability to form brain metastases.
Through the brain windows, they captured images of how these tumor cells migrate to and occupy vascular niches within the brain — sites rich in blood vessels that create microenvironments that affect the behavior of certain cells — discovering quiescent or sleeping cells are drawn to a particular locale: astrocyte endfeet.
Astrocytes are the most common cell in the central nervous system; their endfeet are specialized structures that ensheathe the brain’s microvessels, controlling blood vessels and blood flow.
Through various experiments, the research team discovered that a critical component of the blood-brain barrier called laminin-211 that’s deposited by the astrocytes is what keeps dormant tumor cells dormant.
The researchers found the brain’s normal signaling is “coopted” by disseminated tumor cells in vascular niches containing astrocytic endfeet and this induces signaling that steers them into their quiescent state. As micro-metastases start to proliferate, astrocytes and their endfeet are then stripped from the brain’s vessels.
What triggers this? Ghajar said that’s an unknown for now, calling it a “classic chicken/egg problem.”
“We looked at brain metastasis from 24 different people, including brain mets from patients who’d died. And in each of those metastatic tumors, the astrocytes are gone, the astrocytic protein is gone and there are proliferative tumor cells around it,” Ghajar said. “Does a cell proliferate and as it does it destroys this axis, or does the axis get compromised which allows growth? My guess is either, depending on the situation. We can show the correlation in a human, but not cause. But we could show cause in a mouse.”
A window of opportunity
In addition to pinpointing the cellular mechanics of dormant tumor cells in brain tissue, the researchers also learned that the mechanism is unique.
“One of the major points of the study is that this process is very specific to the brain,” Ghajar said. “The mechanism does not seem to exist anywhere else.”
The bottom line? Now that they’ve located this vulnerability, they can work on ways to target the seeds of brain mets before they have a chance to sprout.
“Tumor cells need to invade, to get into the bloodstream, get out of the bloodstream, to survive in the organ they’re trying to colonize,” Ghajar said. “People have always focused on the ability of these cells to survive. They thought their ability to survive was the rate-limiting step.”
This data, Ghajar said, shows that the bottleneck to brain metastasis is not cells gaining entry to the brain or surviving once there. Instead, the research definitively points to escape from dormancy as the rate-limiting step.
And that presents a window of opportunity.
“What we want to do ultimately is target the dormancy phase,” Ghajar said. “We have real evidence that this is what limits metastasis. If we could keep things in this state, or if we could eliminate them while they’re in the state, that would help prevent metastasis. Now we just have to figure out the precise way to do this. Stay tuned!”
In Research and Cancer Care, Indigenous Representation Matters
Fred Hutch, UW researchers work to reduce risk and inequities and improve access to care, resources for Indigenous communities and patients
 Dornell Pete’s grandparents were both diagnosed with lung cancer, although neither of them smoked.
Dornell Pete’s grandparents were both diagnosed with lung cancer, although neither of them smoked.
“My grandfather worked in the mines, inhaling the uranium in the air, then came home where my grandmother would wash his clothes, so she was also exposed,” said the University of Washington Navajo (Dine’) doctoral student, who grew up in Shiprock, New Mexico, on the Navajo Nation.
Read more
Pete experienced health inequities firsthand growing up: shortages of clean water, fresh healthy foods and reliable health care for those living on reservation lands. Later, as a college undergrad and caretaker for her aging grandmother, she learned how to push back, ensuring the U.S. government would compensate her grandparents (uranium mines were built on tribal lands and Navajo mine workers were routinely exposed to harmful levels of the toxic metal without knowledge, consent or protective gear).
“There were many differences in education and resources growing up,” she said. “Some people had things and other people didn’t.”
These lived experiences are what led Pete to pursue advanced degrees in public health and epidemiology. Her goal: to get to the heart of the health issues the Navajo people faced — issues like diabetes, mental health, suicide, infectious diseases and cancer — and help turn things around through community-engaged research.
“In the Navajo teachings this is something you do,” she said. “You give back. You come back to the family and the community.”
Pete and other Native American advocates, researchers and scientists within the Fred Hutch/University of Washington Cancer Consortium are giving back to science and public health as well, conducting research with American Indian/Alaska Native individuals and communities that could lead to longer and healthier lives for all.
‘Walking in both worlds’
“Representation is really important; it plays a vital role in cancer prevention and research,” said Craig Dee, also a member of the Navajo (Dine’) Tribe, and a community health educator with the Cancer Consortium’s Office of Community Outreach & Engagement.
But it’s not just representation within the health care system, he said.
“There also needs to be representation at the research level, at the principal investigator level in cancer and prevention research,” said Dee, who is pursuing a master’s degree in public health at UW. “The community needs to see commonality and your understanding of the lived experiences that stream from historical trauma and colonization. This helps with the trust.”
Originally from the Four Corners region, Dee focuses on urban American Indian and Alaska Natives, which he terms an “often-overlooked population.”
Like Pete, who recently received a large grant from the National Cancer Institute to study stomach cancer risk among the Navajo people, Dee works to connect two communities — academic and Indigenous.
“My work is to walk in both worlds,” he said. “To build relationships and create internal and external educational opportunities, but lately more so to support the scientific community to better understand and acknowledge the significant value of Indigenous relationality in cancer research.”
Dee said strengthening the health of American Indian and Alaska Native peoples means recognizing research and data evaluation as Indigenous values that can be used to tackle the health disparities they face.
“American Indian and Alaska Natives have been observational researchers since time immemorial,” he said. “A lot of our traditional medicines, ones that were used thousands of years ago to treat infection, relieve pain and other things, are still being used today.”
Storytelling and science
Information about these medicines was passed along — not through scientific publications — but oral storytelling, which still provides value today.
Listening to people’s stories is how Pete learned of the cancer burden in her community, including the fourfold rate of stomach cancer in Navajo people compared to the surrounding population.
“As an epidemiologist, your training is to find out how much of a burden there is and that starts with stories, with people talking about cancer,” she said. “Stomach cancer was one no one expected. But among Native people in the Southwest and also among the Alaska Native population, the stomach cancer disparity is high.”
As principal investigator of the Assessing the Gut Microbiota and Individual Diet (or ‘ABID study — “Abid” is the Navajo/Dine’ word for stomach), Pete hopes to find the root of this disparity and is gathering data on the prevalence of infections with the bacterium H. pylori, a strong risk factor for stomach cancer.
“Prevention is where my heart is,” she said. “And most people don’t realize there’s a link between infectious disease and cancer.”
Done in collaboration with Hutch researcher Dr. Amanda Phipps, it’s one of only a few studies to look at this risk factor among members of the Navajo Nation. And it wouldn’t have happened without Pete.
“Working with Dornell has been hugely educational,” Phipps said. “She’s very much attuned to the needs of the community and also how things are done. You don’t just walk into Navajo Nation and expect to conduct research without support and buy-in. She talked with community leaders, with folks from the IRB [the Institutional Review Board, which governs research] and the health care systems on the Navajo Nation to hear from them what the challenges were. She made sure all of them had their voices heard in the research process.”
Representation and collaboration, Phipps said, are crucial for effective cancer prevention.
“Public health includes the public in it,” she said. “It is a science that involves the public and should not be removed from the people we’re hoping to serve with the science we produce.”
And public health has long been part of American Indian/Alaska Native cultures, Dee said.
“Indigenous people have always been involved in public health,” he said. “One of the things we’re taught within my community is if there’s an elder who needs help, then you help that elder like she’s your own grandmother, like a blood relative. That’s a shared teaching and value among Indigenous communities. We look out for the community and looking out for the community is public health, making sure our elders, our children, our women, our community are safe.”
A higher burden of disease
And there is much to keep these communities safe from, particularly in the realm of cancer.
Data from the National Cancer Institute shows that American Indian/Alaska Native populations have the lowest survival rates for nearly all types of cancer of any subpopulation in the U.S., possibly because these cancers are often detected late, when they are harder to treat. National data from the Centers for Disease Control and Prevention tell us:
- American Indian/Alaska Native people are more likely to get liver, stomach, kidney, lung, colorectal, and female breast cancers than white people in most regions.
- American Indian/Alaska Native men have higher rates of myeloma and liver, stomach, kidney, colorectal and lung cancers than non-Hispanic white men.
- American Indian/Alaska Native women have higher rates of liver, stomach, kidney, colorectal and cervical cancers than non-Hispanic white women.
- Additionally, the federal government’s Office of Minority Health has found that American Indian/Alaska Native men are twice as likely to die from stomach cancer once they’re diagnosed and American Indian/Alaska Native women are 2.2 times more likely to die from liver and bile duct cancer once they’re diagnosed.
In Washington state, Fred Hutch/UW Cancer Consortium data show American Indian/Alaska Native people are diagnosed with breast cancer at 1.6 times the national rate and blood cancers at nearly twice the national rate.
Before vaccines became available, COVID-19 hit Indigenous communities harder, as well.
“Rates of COVID-19 for American Indian and Alaska Native communities were 3.5 times higher than they were for non-Hispanic whites,” Dee said, adding that the numbers do not account for racial misclassification.
Trauma, abused trust, and toxins
What leads to the higher rate of disease in Indigenous people? According to research, it’s multifactorial. And as with African Americans, much of it starts with persistent racial inequity and trauma, historical and otherwise.
“Seven out of 10 American Indian/Alaska Native people live within large urban areas,” said Dee. “This is due to either moving or being forced to relocate because of government policy, lack of economic and educational opportunities, and/or limited access to health care and other services.”
Additionally, over decades, tens of thousands of Indigenous children in the U.S. and Canada were separated from their families and forced to live in residential schools designed to “kill the Indian … save the man.” Subjected to enforced assimilation, they had to abandon their language, clothing, food and customs and were routinely beaten, abused, sickened by disease and worse.
Many Native families and individuals still carry trauma from this. And it’s hardly ancient history. The practice didn’t end until passage of the Indian Child Welfare Act of 1978. There is ongoing trauma, as well, including that from the high numbers of missing and murdered Indigenous women and girls in the U.S. and Canada.
Other contributing factors include inadequate medical facilities on reservation lands, shortages in health care providers and lack of access to preventive screenings.
“Cancer screenings are low in Indigenous people,” Pete said. “The Navajo Tribe does have a breast and a cervical cancer screening program, but screenings for other cancers like lung and colorectal need improvement. With cancer, it’s about access to care. It’s about who gets access to screening, clinical trials and good therapies, including effective cancer prevention programs.”
Environmental exposures from polluted air, water and soil and/or toxins from manufacturing plants and mines built on or near tribal lands, like the one Pete’s grandfather worked in, have increased health disparities. Ditto for isolation and lack of transportation.
“My grandfather was advised not to treat his lung cancer because of his age,” Pete said. “But it was also that we couldn’t travel two hours to get treatment and surgery and then come back and follow up with his care. There are geographic problems and lack of specialty care. We have to seek care off the reservation and in particular environments, racism is present in terms of our treatment.”
Language barriers can also impede care.
“A lot of people speak their tribal language, so there may be a lack of understanding between provider and patient,” she said. “There’s no word for cancer in our tribal [Navajo/Dine’] language.”
Another complicating factor is tobacco use.
“It’s high and a problem in our catchment area [the 13 Puget Sound counties that the Fred Hutch/UW Cancer Consortium serves],” said Ursula Tsosie, program manager and tribal liaison for the Indigenous health promotion program at Seattle Cancer Care Alliance, the Hutch’s clinical-care partner.
“American Indian and Alaska Natives smoke twice as much as other people,” she said. “In non-Indigenous people, prevalence is like 15%, but for our Native groups, it’s like 32%. They have a high number of quit attempts, but also high relapse. So they’re trying to quit; it’s just hard. What we’ve found in our conversations with communities is that it’s about trauma. It’s about coping.”
Working with tribes to cut tobacco use
Hutch public health researcher and behavioral psychologist Dr. Jonathan Bricker, who just published a study on smoking cessation in American Indian and Alaska Native people, said the high rates of cigarette use in this population is a combination of internal and external factors.
“There’s historical trauma, which is the psychological wounding of a group across generations, there’s racism, and there’s also the ceremonial use of tobacco in certain tribes,” he said. “Tobacco companies have also exploited tribes’ sovereignty from smoke-free laws with promotional strategies. And lack of access to cessation treatment (due to costs and living remotely) is a major barrier that keeps smoking rates high.”
Bricker’s study included American Indian/Alaska Native participants from 31 states, with 70% of them in urban areas and 30% residing on reservation lands. Funded by the NCI with additional help from the local Snoqualmie Tribe, his findings showed that a digital intervention with the ICanQuit smartphone app, using Acceptance and Commitment Therapy, was twice as effective in helping this population quit smoking as compared to a standard NCI quit-smoking app.
“ICanQuit shows exceeding promise in effectively addressing these causes and barriers to treatment,” he said.
And it’s not the only program designed to help Indigenous people kick cigarettes.
SCCA established the həliʔil Program (pronounced haa-lee-eel) in 2019 to promote lung cancer screening and cessation of commercial tobacco products in Indigenous communities. The name “həliʔil” (a Lushootseed word meaning “to become well and heal”) was also gifted to SCCA by the Snoqualmie Tribe.
Tsosie, also a member of the Navajo (Dine’) Tribe, said the program is developing a culturally appropriate lung cancer screening navigation program. They also offer trainings to SCCA staff and providers in order to better serve patients who identify as Indigenous.
Navigating cancer care
SCCA also has its own Indigenous patient navigator, Lenora Starr, who serves American Indian/Alaska Native as well as Native Hawaiian populations.
“I‘m very grateful that SCCA has been able to hire Indigenous persons to work on both the prevention and the navigation side of cancer,” Starr said. “I like to think we’re making a difference in being able to identify and reach out to people, whereas before, they might slip through the cracks.”
A member of the Confederated Tribes of Warm Springs in Oregon, which represents a handful of Northwest tribes, Starr has also experienced health inequities over the years. Her former partner, for instance, repeatedly saw doctors about gastrointestinal issues but was never helped. Instead, he was told he wasn’t able to eat because of anorexia.
“He actually had colon cancer,” she said. “But it wasn’t found until he was stage 4. There was a huge delay. He died shortly after he was diagnosed.”
As patient navigator, Starr meets with newly diagnosed patients and families who identify as Indigenous, assisting them with whatever services or comforts they may need, whether it’s connecting them with transportation, lodging, counseling services or financial resources; or teaching visiting relatives how to use Seattle’s bus system. She’s even brought a homesick coastal patient some canned salmon from her pantry.
“Some people will say they don’t want help or they’ll say they’re okay, but then when they find out I’m Indigenous they’ll open up more,” she said. “When I tell them it’s part of my job to look for grants and financial assistance for patients, they’re more receptive.”
Starr also works with Indigenous patients and communities to help them understand the important difference between ceremonial and commercial tobacco use (ceremonial tobacco has no chemical additives).
‘A silver lining’
Despite the challenges in Indigenous health and research, Pete, Dee and the others are not at all discouraged.
“The pandemic shined a light on the inequities across all systems, especially for people of color,” Pete said. “But there’s a silver lining. It’s made us more passionate. COVID has put a fire in us to look at the data and see the disparities and go after the funding and research to change it. And to get more education about disparities back to our people.”
Outreach efforts during the pandemic made a huge difference in vaccination uptake, the researchers said. At this point, American Indian/Alaska Native people are leading the U.S. in vaccination rates. Dee said he believes the Indigenous values of protecting communities was a large factor.
“I think it’s a matter of our tribal communities being diligent about caring for the people and caring for our elders, the knowledge-keepers,” he said.
In the future, Pete said she hopes to use technology and other tools in similar ways to disseminate information on cancer and cancer prevention and to demystify cancer screenings.
“I’m very interested in getting out of the ivory towers,” she said. “There are other populations that can benefit from this research and this work.”
Dee couldn’t agree more.
“It’s critical that we share this knowledge and engage with the research and academic communities on behalf of our people and relatives,” he said. “This is what representation looks like.”
 Join the Thomas Legacy Society
Join the Thomas Legacy Society
The Thomas Legacy Society at Fred Hutch is a special group of supporters who have made a commitment through a legacy gift to drive lifesaving cancer research and improve the lives of patients in the years to come.
What does a unique gift like this actually do? By making a gift for Fred Hutch in your will or trust, or by naming us as beneficiary on one of your financial or investment accounts, you contribute to:
- Research for discovering how to prevent, detect and treat cancer and related diseases.
- Upgrades to existing technology and acquisitions of new equipment.
- A variety of assistance and support for patients and their families.
- Staff and researchers who further the cause of curing cancer faster.
Visit our website to learn more or contact us.
Already included Fred Hutch in your estate plans? Please let us know so we can ensure your wishes are carried out as you intend!
Important Update
Fred Hutchinson Cancer Research Center and Seattle Cancer Care Alliance have merged, creating an organization that aims to bring scientific advances to patients faster, and deepens longstanding ties with UW Medicine.
Under the restructuring formally launched on April 1, Fred Hutch and SCCA are united as a single, independent, not-for-profit organization now called Fred Hutchinson Cancer Center (Tax ID: 91-1935159). The unified organization will be a clinically integrated part of UW Medicine and UW Medicine’s cancer program.
“Today’s milestone is a tremendous step toward our vision of decreasing the time between discovery and delivery of the most advanced treatments for our patients,” said Fred Hutch President and Director and Raisbeck Endowed Chair holder Dr. Thomas J. Lynch, Jr., who held the same titles at Fred Hutchinson Cancer Research Center before the merger. Read more about it here. Questions on how our merger affects your estate plans? Contact the planned giving team.
