Fred Hutch Legacy Insiders
Loyal supporters and their advisors are helping to accelerate discoveries that prevent, treat and defeat cancer and infectious disease. We invite you to learn about the innovative breakthroughs their support makes possible.
Legacy Gratitude Luncheon: Inspiration and Impact
Celebrating Fred Hutch supporters and their commitment
 Fred Hutchinson Cancer Center was delighted to host our Legacy Gratitude Luncheon on March 30. The event brought together 150 Fred Hutch supporters, including Thomas Legacy Society members (supporters who have made a commitment through a gift in their will, trust, or other planned gift), monthly donors, longtime volunteers, and 10-year participants in Obliteride, our annual summer bike ride and 5K. We were honored to celebrate the many ways our supporters commit their powerful intentions to Fred Hutch.
Fred Hutchinson Cancer Center was delighted to host our Legacy Gratitude Luncheon on March 30. The event brought together 150 Fred Hutch supporters, including Thomas Legacy Society members (supporters who have made a commitment through a gift in their will, trust, or other planned gift), monthly donors, longtime volunteers, and 10-year participants in Obliteride, our annual summer bike ride and 5K. We were honored to celebrate the many ways our supporters commit their powerful intentions to Fred Hutch.Read more
We build our legacy upon what we learn, the relationships we form, and the difference we’ve made in peoples’ lives. Fred Hutch’s loyal donors and volunteers share a commitment to accelerating lifesaving research that can improve outcomes for people facing cancer and other diseases. This commitment, in all the ways it comes to life, makes a tangible difference in our community.
Memorable remarks and exciting innovation
Examples of supporters’ dedication and extraordinary impact were on display throughout the lunch.
Over entrees, Nancy Greenwood Vehrs, assistant vice president of Philanthropy, spoke about her own connection to our mission. Nancy began her work with Fred Hutch soon after her husband died of lymphoma. First as volunteer, then as a staff member and annual donor, and now also a proud member of the Thomas Legacy Society, Nancy’s engagement continues to evolve. For the last 10 years, Nancy has also been an ardent Obliterider, and she shared what it means to have loved ones join her for that special August experience. “Last summer, all seven of my grandchildren participated in Obliteride with me,” she said. “It is a joy to see that generation learning about how good it feels to give back.”
Thomas J. Lynch Jr., MD, president and director and holder of the Raisbeck Endowed Chair, then discussed the future of cancer care with William “Bill” Grady, MD, a physician and professor at Fred Hutch and UW Medicine and medical director of Fred Hutch’s Gastrointestinal Cancer Prevention Program. The two highlighted the importance of screening for colon cancer, noting that while colonoscopy is best, any screening is better than no screening. They also commented on the many efforts underway to help more people get screened for GI cancers.
Thank you
It was amazing to see so many of you at the Legacy Gratitude Luncheon! We were honored to celebrate the legacy you have created with us by helping us pursue scientific breakthroughs and healthier lives for every person in every community. For those who could not attend, we hope to meet with you soon to extend our gratitude and share more about the exciting work happening here at Fred Hutch.
If you are considering including us in your will, trust, or other financial documents, please let us know so that we can include you in our Thomas Legacy Society and recognize your investment in the future of Fred Hutch. We also invite you to join us in Obliteride this year and explore other ways to support Fred Hutch.
To learn more, please contact Renee Kurdzos, executive director, Planned Giving, at rkurdzos@fredhutch.org.
Obliteride unites community for cancer cures
Registration opens for Fred Hutch’s summer bike ride, 5K fundraiser
 Join the fight against cancer at Obliteride, Fred Hutch Cancer Center’s annual bike ride and 5K fundraiser. Participants can bike 25-100 miles, walk/run the 5K, or volunteer in support of this cause. There are discounts for those who have had cancer, fundraising tools and a kickoff party with live music and catered dinner. Since 2013, Obliteride has raised over $40 million to fund cancer research and compassionate care. Read more about this event below!
Join the fight against cancer at Obliteride, Fred Hutch Cancer Center’s annual bike ride and 5K fundraiser. Participants can bike 25-100 miles, walk/run the 5K, or volunteer in support of this cause. There are discounts for those who have had cancer, fundraising tools and a kickoff party with live music and catered dinner. Since 2013, Obliteride has raised over $40 million to fund cancer research and compassionate care. Read more about this event below!Read more
Registration is now open for Obliteride, Fred Hutchinson Cancer Center’s summer bike ride and 5K fundraiser slated for Saturday, August 12, in Seattle, Wash.
This annual community event brings together people from around the Pacific Northwest (and beyond!) to help cure cancer faster by raising vital research funds. Every participant-raised dollar fuels advances in cancer prevention, detection, treatment and cures that improve and save lives.
Participants can sign up to bike either a 25-, 50-, or 100-mile route, walk or run a 5K, or volunteer along with thousands of other passionate community members. Registration discounts are available for all those who have or have had cancer. There will also be a virtual option for those who can’t join in person.
Exciting opportunities for 2023
“This year, Obliteride participants may direct their fundraising to the areas that are most meaningful to them, including a specific disease area, program, faculty member or clinician,” said Kelly O’Brien, vice president of philanthropy at Fred Hutch. “With this new option, this dedicated community can rally their friends and families to support the work they care about most.”
A new fundraising guide, updated tools and customized support will help every Obliterider meet their fundraising commitments, she said.
In addition, updated bike routes will take riders by beautiful lake views and through a variety of different terrain. Riders on the 100-mile route will enjoy lunch at Carnation Farms in Carnation, Wash. Walkers will have a paved, family-friendly route.
The event will once again include a kickoff party the night before (August 11) at Gas Works Park near the Fremont neighborhood in Seattle. The party will include a catered dinner, live music and the opportunity to connect with a community dedicated to cancer cures.
Obliteride fundraising goes directly to work
As in previous years, 100% of participant-raised dollars will help advance lifesaving research and compassionate care at Fred Hutch, thanks to generous sponsors.
Since 2013, Obliteride has raised more than $40 million and fueled more than 200 projects, including new approaches for breast, colon, pancreatic and prostate cancer; novel therapies that harness immune T cells to fight lung and skin cancers; breakthroughs in data science; advances that help distill complex genetic and environmental factors to better predict disease risk; community partnerships to improve health and more.
Register today! Ride, walk, run or volunteer this August and help cure cancer faster.
Improving immunotherapy for advanced prostate cancer
Preclinical work identifies better target and recruits more immune cells to make CAR-T therapy work for solid tumors
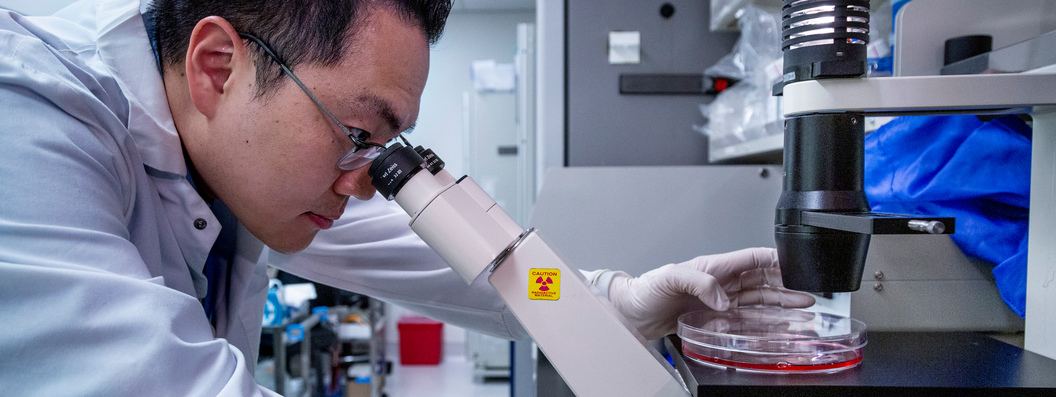 CAR-T cell therapy holds great promise as an effective treatment for advanced prostate cancer. By combining this cutting-edge, engineered treatment with molecules that recruit host immune cells, researchers have shown remarkable success in delaying tumor progression and extending survival time. With additional testing and research, this combination approach could revolutionize treatments for many types of solid tumors — and pave the way towards a future of better, more effective cancer care.
CAR-T cell therapy holds great promise as an effective treatment for advanced prostate cancer. By combining this cutting-edge, engineered treatment with molecules that recruit host immune cells, researchers have shown remarkable success in delaying tumor progression and extending survival time. With additional testing and research, this combination approach could revolutionize treatments for many types of solid tumors — and pave the way towards a future of better, more effective cancer care.Read more
Picking the right target and helping recruit a wider range of anti-tumor immune cells can help improve CAR-T cell therapy against advanced prostate cancer, according to new preclinical work from Fred Hutchinson Cancer Center scientists, published in Nature Communications earlier in April. The newly developed CAR-T cells described in the study will form the basis of an early-stage clinical trial to test them in people whose late-stage prostate cancer has defied other treatments.
“This is the first time this approach has been applied to prostate cancer and in the context of engineered T-cell therapy,” said Fred Hutch prostate cancer researcher John Lee, MD, PhD, who led the study. “We showed applying this immune-boosting drug to an immunologically ‘cold’ tumor microenvironment can convert it to a hospitable, ‘warm’ environment.”
Lee’s team developed an engineered chimeric antigen receptor (or CAR) T-cell therapy directed against a molecule called STEAP1, which is expressed more uniformly across tumor cells from advanced prostate cancer than the more commonly explored target, PSMA, or prostate-specific membrane antigen. The group showed that when anti-STEAP1 CAR T cells were combined with a drug developed by collaborators at Imperial College London that focused an immune-boosting molecule within tumors, the CAR T cells could more effectively reduce prostate tumor growth and progression in preclinical models of the disease. The strategy also helped prevent the tumors from escaping immune attack by drawing in host T cells that could attack a wider range of targets.
The anti-STEAP1 CAR T cells that Lee and his team developed are already tailored for use in people. Supported by the National Cancer Institute Experimental Therapeutics Program, or NExT, the team will test their newly anti-STEAP1 CAR-T cells against metastatic, “castration-resistant” prostate cancer in a Phase 1 clinical trial slated to open in early 2024.
Prostate cancer: a challenge for engineered immune cells
In the last decade, new treatments that block the androgen receptor and its downstream effects have extended the lives of men with advanced prostate cancer — but eventually metastatic prostate tumors evolve to resist these therapies. People with advanced, so-called “castration-resistant” prostate cancer desperately need therapies that can attack this disease, and Lee is hunting for them.
One avenue that Lee and other prostate cancer researchers are exploring is immunotherapy. Immunotherapies have been transforming cancer treatment: checkpoint inhibitors for once-deadly melanoma and non-small cell lung cancer, and engineered immune cells for various types of leukemia and lymphoma. Prostate cancer was the first cancer type to get a specialized immunotherapy when the cancer vaccine Provenge (sipuleucel-T) was approved to treat asymptomatic metastatic castration-resistant prostate cancer in April 2010. Lee aims to capitalize on these advances to develop new, immune-based treatments that will treat, or perhaps even cure, these deadly cancers.
He focuses on engineered immune cells known as T cells, that carry a scientist-designed molecule called a chimeric antigen receptor, or CAR, that can help them find cancer cells to kill. Memory T cells can live as long as the person carrying them — making them a potentially powerful weapon against cancer and recurrence.
“We started with the idea that we might be able to leverage the potency of memory T cells as a living drug,” Lee said.
Solid tumors like prostate cancer make it tricky for scientists to effectively deploy engineered T cells. The best CAR-T target needs to be found almost exclusively on tumor cells to minimize killing of healthy tissues and uniformly on tumor cells — to reduce the chances that tumor cells will escape the T-cell onslaught. The CAR T cells currently on the market target cells with a protein called CD19 on their surface. These CARs work against B-cell malignancies — leukemias and lymphomas — and they take advantage of the fact that only B cells carry CD19.
These kinds of targets are difficult to find on solid tumors like prostate cancer: many of the proteins they express are found elsewhere in the body, and oftentimes, even if a protein is found primarily in a tumor, many tumor cells still won’t have it.
To make Lee’s and other immunotherapy researchers’ jobs even harder, the microenvironment of solid tumors often changes to tamp down immune attack. Tumors may keep T cells out by releasing less molecules that attract them. Other immune cells that do get into the microenvironment may get “turned,” switching to a pro-tumor mode that allows them to shut down activity of T cells that do find their way into the tumor. Such tumors are termed immunologically “cold” because they prevent ignition of the inflammatory environment T cells need to do their jobs.
To develop an effective anti-prostate cancer CAR-T cell therapy, Lee needed to overcome both hurdles: find the right target, and “thaw” the tumors.
Seeking STEAP1
Prostate-specific membrane antigen, or PSMA, is highly expressed on prostate tumor cells, and forms the basis for a variety of diagnostic tests and treatments. Other scientists are working to develop CARs that target PSMA, but Lee’s studies suggested that prostate tumors might harbor even better CAR-T targets.
In 2018, his team found that a protein called STEAP1 is among the most highly enriched proteins on the surface of prostate adenocarcinomas, the most common type of prostate tumor. Other researchers have also linked STEAP1 to cancer, and tried to develop immunotherapies aimed at STEAP1, like the antibody-drug conjugate vandortuzumab vedotin, though none have cleared early-stage clinical trials. In the current Nature Communications study, Lee’s group, led by postdoctoral fellow Vipul Bhatia, PhD, dug deeper into STEAP1 expression in prostate tumor cells, and compared it to PSMA.
They surveyed STEAP1 on prostate tumor biopsies from men who had donated their tumor tissue through the University of Washington/Fred Hutch prostate cancer rapid autopsy program. They found that in addition to occurring at high levels on prostate tumor cells, STEAP1 was also found on a much higher proportion of prostate tumor cells than PSMA. And, when they looked at prostate tumor tissue biopsies taken from more than one metastasis in an individual patient, the researchers saw that STEAP1 was found across metastases — suggesting that many prostate tumor cells would be vulnerable to a STEAP1-targeting treatment.
CARs are a mash-up of an antibody and the molecular apparatus T cells use to detect and propagate signals through the T-cell receptor, the molecule T cells usually use to determine which cells to target. Bhatia built his new CAR using the antibody originally developed for the antibody-drug conjugate that had foundered in a Phase 1 trial, likely due to the toxicity of the drug attached to the antibody. He fused this to a second-generation CAR backbone that incorporates the latest constituents that promote T-cell persistence and activation.
The CAR that Bhatia and Lee developed allowed T cells to recognize cells that bear STEAP1 — even at very low levels, helping to increase the number of prostate tumor cells likely to be vulnerable to the therapy.
Finding an effective combo against prostate tumors
To test the new CAR T against prostate cancer, Lee and his group used patient-derived xenograft (or PDX) models, in which tissue taken from human prostate tumors is grown in mice. Bhatia injected the anti-STEAP1 CAR T cells into prostate tumors and saw significant inhibition of tumor growth over 25 days.
In a preclinical model of metastatic prostate cancer, mice that didn’t receive engineered T cells lived on average 31 days. A dose of CAR T cells delayed tumor progression and extended survival to 97 days. In a separate model of metastatic castration-resistant prostate cancer, the engineered T cells appeared to cure the mice. The team also developed mice that expressed a “humanized” version of STEAP1 to test both efficacy and safety of the strategy. In these mice, the engineered CAR T cells doubled survival time, but even though tumors initially shrank, they quickly relapsed and began to grow again. The engineered T cells didn’t appear to cause damage to other organs.
Bhatia and Lee’s investigations showed that when tumors progressed during CAR-T cell treatment, they did so by reducing STEAP1, the CAR target. They found that reducing STEAP1 also appears to help tumor cells become invisible to host T cells that don’t carry a CAR, as these cells also ramp down the molecules T-cell receptors use to detect targets.
While the CAR-T treatment was initially effective, the tumors went cold to escape it. To find a way to warm up the tumors, Lee turned to bioengineer Jun Ishihara, PhD at Imperial College London. Ishihara had developed collagen-binding domain-IL-12, or CBD-IL-12, a modified version of the immune-boosting molecule IL-12 fused to a piece of protein that binds to collagen.
“When you give this fusion protein systemically, it goes to areas of disordered vasculature where collagen is exposed — which is cancer,” Lee said.
This allows IL-12’s immune-inflaming activity to concentrate exactly where it’s needed. Bhatia tested the combination of anti-STEAP1 CAR T cells plus an intra-tumor dose of CBD-IL-12 in two PDX models of prostate cancer that respond poorly to checkpoint inhibitor therapy. (Checkpoint inhibitor therapy acts to block molecular “brakes” or inhibitors that keep T cells from attacking their targets.)
When closely examined, the injected tumors showed signs of a warmer, more immune-welcoming environment than uninjected tumors, including higher levels of the molecules involved in marking cells for T-cell attack.
In a model of metastatic prostate cancer, the combination of the engineered T cells and weekly CBD-IL-12 injections significantly delayed tumor progression and extended survival compared to either CBD-IL-12 given with unengineered T cells (“blind” to STEAP1-bearing cells) or engineered T cells alone.
Not only did the warmer tumor microenvironment help the CAR T cells act more effectively, but Bhatia found that it helped recruit host immune cells. This means that there’s a wider range of molecules being targeted by the immune system, which makes it harder for tumors to evade attack, even if they do find a way to tamp down STEAP1.
“We found that this combination is more effective in controlling the disease, but it’s not a cure-all,” Lee cautioned.
Testing the approach in the clinic
Lee and his team are gearing up for an early-stage clinical trial that will test their new CAR T cells against advanced prostate cancer. The team’s preclinical results are promising enough that the NCI is partnering with the team to get it to patients and NExT will produce the engineered CAR T cells needed.
The Phase 1 trial will test safety and some degree of efficacy of the anti-STEAP1 CAR T cells against advanced prostate cancer, though more testing is needed before a combo CBD-IL-12/CAR T strategy makes its debut in people. Lee and Bhatia’s CAR T cells incorporate leading-edge advances developed at Fred Hutch known to help make CAR-T therapy more powerful and longer lasting, including engineering T cells with an ideal percentage of memory-type T cells that can form the basis of a longer-lived response.
Lee thinks that the basic strategy described in the Nature Communications study — boosting the reach and power of CAR T cells with other molecules that recruit host T cells — could one day be adapted for other “cold” solid tumors. And his CAR T may be relevant to other tumors that are known to express STEAP1, such as Ewing sarcoma, a cancer of the soft tissue that usually arises in childhood or adolescence.
His team is also working to extend and optimize the combo approach, he said.
“We want to empower not only the CAR T cells, but also we’re trying to empower the host immune system to aid and fight against the cancer,” Lee said. “Those studies are ongoing, but they’re really promising.”
This work was supported by the Department of Defense Prostate Cancer Research Program, Swim Across America, the Pacific Northwest Prostate Cancer SPORE, the Institute for Prostate Cancer Research, a Fred Hutch/University of Washington Cancer Consortium Safeway Pilot Award, the Doris Duke Charitable Foundation, a JSPS Overseas Research Fellowship and the Prostate Cancer Foundation.
Dedicated supporters at the Heart of the Hutch
Using creativity and passion to support Fred Hutch research in good times and bad

One family’s tragedy has become a powerful force for good, as Richard and his family have turned their pain into a passion for finding a cure for melanoma. By creating BOWL-A-NOMA, they have mobilized a supportive community of volunteers to donate funds to further research into cancer treatments and prevention. They are an example of how it is possible to turn heartbreaking loss into the hope of saving lives.
Read more
Bowling to honor a son — and “strike out” melanoma
“Our tagline is ‘Strike Out Cancer, Spare A Life’,” said BOWL-A-NOMA co-founder Richard Hull. Each May, the bowling event and party, created in honor of his late son, Elliott, unites a dedicated community to raise funding and awareness for melanoma research, including at Fred Hutchinson Cancer Center.
“Today happens to be Elliott’s — what would have been Elliott’s 40th birthday,” said Richard, on a call from his home in Seattle, Washington, in early April. Elliott passed away in 2018 at the age of 35, four months after being diagnosed with an aggressive type of skin cancer. He left behind a wife, a two-year-old son and a dedicated community of friends and family.
“By the time he was actually diagnosed, there was little to nothing [his doctors] could do other than try,” said Richard. “So, they tried, and they were not successful. And his ‘You’ve got six months to live’ turned into four.… I had had a conversation with Elliott prior to his passing. And I just felt that in order to preserve my soul, I needed to do something to divert the loss into gain. I came up with BOWL-A-NOMA, a contraction of Bowling and Melanoma.”
Transforming loss into action
Motivated by a mission to honor Elliott’s life, support research into the diagnosis and treatment of melanoma and help others facing the disease, Richard, his wife Louise, and Elliott’s sister Amelia quickly ramped up their efforts. They gathered their community, created a website and registered as a nonprofit. On May 19, 2019, a day officially proclaimed “BOWL-A-NOMA Day” by then Seattle Mayor Jenny Durkan, they invited friends and family to hit the lanes in Seattle for their first annual fundraiser. BOWL-A-NOMA took flight.
Now in its third year (with a pandemic pause in 2020 and 2021) the event will welcome participants from as far away as Pasadena, CA and Girdwood, AK to get involved on Saturday, May 20, at West Seattle Bowl, and make a difference for melanoma research. “Spectators [who would like] to be part of the event with their donations are also welcome to attend,” said Richard.
“It’s always the third Saturday in May,” he adds. “We chose May because it is National Skin Cancer Awareness month.”
Able and willing
BOWL-A-NOMA is a true community effort, said Richard. From volunteers and donors to web designers and musicians, the event relies on the heart of many people. He even enlisted the help of a “very dear” college friend, who designed BOWL-A-NOMA’s signature logo. “In order to maximize all donations from our community of supporters, we do not pay those interested in our cause to come in and do A, B, or C,” he said. “It’s all volunteer work.”
With that support, Richard and his family were able to make their first philanthropic grant in 2022: a generous donation of $50,000 to the laboratory of Kevin Barry, PhD, a researcher and assistant professor at Fred Hutch. Dr. Barry’s team is exploring new ways to harness the immune system to attack melanomas and protect patients.
“We chose Fred Hutch because they are the most notable cancer research center in the northwest, and perhaps in the nation,” said Richard.
Last year, the Hull family visited Fred Hutch’s Seattle campus to tour the Barry Lab and talk with the team. “I think it might have been Louise that asked [Dr. Barry], Why do you do this work?” said Richard, “And he said, ‘Because I’m able and willing.’ And that really stuck with me, because almost everybody that I know is capable of doing a lot.”
When he talks to his community, Richard said he doesn’t just ask people to donate but to support the mission by sharing it with everyone they know.
“Are you willing to go out into your community of peers, be they friends, family, coworkers, associates, neighbors, whatever, and share our ‘gospel’ so that we can grow our community?” he asks. “I know you’re capable of doing that.”
Breakthrough science to improve lives
Dr. Barry said that the Hull family’s visit was deeply moving for his team.
“When I met Richard and Louise, I was struck by the love that they have for Elliott and the pain they feel from his loss. Our meeting was a powerful reminder about why we do this research. The Hull family is a prime example of what motivates our research group to pour our energy into pushing for a future where we have prevention, treatments, and cures for melanoma and other cancers. The support and personal commitment of the Hull family and their community help make this possible.”
Last May, Dr. Barry and members of his team also attended BOWL-A-NOMA as speakers and participants — and plan to attend again. “I am incredibly honored to be supported by this community,“ he said.
Bringing it all home
Now, Richard and the BOWL-A-NOMA community are gearing up for their May event, which will feature a 60s-themed party. Fundraising will once again honor Elliott by supporting breakthrough research in the Barry Lab.
“If you look at our BOWL-A-NOMA logo, there’s an element in it that brings it all home,” said Richard. “There’s a black [bowling] ball. On it is the monogram from Elliott’s signet ring that we had made for him when he turned 21. The number one purpose is to keep the spirit of my son Elliott alive. His spirit will definitely be present at BOWL-A-NOMA as we join together on May 20 to Strike Out Cancer and Spare A Life!”
— By Laura Anderson
Join the Thomas Legacy Society
The Thomas Legacy Society at Fred Hutch is a special group of supporters who have made a commitment through a legacy gift to drive lifesaving cancer research and improve the lives of patients in the years to come.
What does a unique gift like this actually do? By making a gift for Fred Hutch in your will or trust, or by naming us as beneficiary on one of your financial or investment accounts, you contribute to:
- Research for discovering how to prevent, detect and treat cancer and related diseases.
- Upgrades to existing technology and acquisitions of new equipment.
- A variety of assistance and support for patients and their families.
- Staff and researchers who further the cause of curing cancer faster.
Visit our website to learn more or contact us.
Already included Fred Hutch in your estate plans? Please let us know so we can ensure your wishes are carried out as you intend!
